Earlier in the year I didn’t appreciate the environment of being around doctors and residents as much as I do now. As a brand new first year, you listen to Pathology Residents in their conferences and think you won’t learn about the same things as the people getting their doctorate degree and you quickly come to find in the program you need to know a lot more than you’d ever believe. I mentioned in my previous post I assisted in an autopsy. A resident and second year really helped and at the end of the case the Pathologist came in to review the organs that were prepared by the team I got to be a part of. I thought when he came in, I would step aside and let him discuss the case with the resident, but he quickly told me to come over as the resident gave her run down of the case, clinical history, and what had been found. We were the ones that saw the case from the external examination to in-situ, to when the sections were submitted by the resident, so we saw first-hand what all was involved. He told me if there was something he says that I don’t understand to stop him and ask, making me feel included and ready to learn as much as I could. As we went on, he asked me questions on the polyp I submitted and asked about what would be in my differential for this case. He went around asking each of us questions about different scenarios and he was ready to give information and make our knowledge applicable. I was excited that I could tell him how I would handle a specimen with a history of a certain cancer if it came in the gross room after a surgeon oriented it. He stopped to explain a lot of things, most of which we had learned in Robbins textbook so yes, I will tell you now reading it and all of those tests in Systemic Path over the summer are worth it when a Doctor asks what you think and you can give a correct answer. I feel as though WVU and the environment they created here with learning from various health professionals really gave me something I didn’t know I was looking for when I was applying to programs. Learning directly from the doctors who have years of experience combined with the PA’s as our professors really sets a student up for success. These professors never put aside their work, just take on the extra responsibility of training medical professionals the right way. If you are coming to the program, remember to learn as much as you can from these people and if you are thinking of applying to PA school think about what the program has to offer you, not just what you offer them. And I’d say this program has a lot to offer.
Raise Your Hand if You’ve Ever Felt Personally Victimized by Covid-19
Mental health is an important topic that I feel like I should talk about for a minute on a blog that students read. I came home today from a lab and assisting in an autopsy and something felt off from the start of the day. In the autopsy there was a resident and a second year PA student and we really got our hands in and prepared the organ blocks for this case. They both helped me a lot and everything I learned in lecture got to come to life today. They showed me how to take sections which are quite different than surgical pathology and one day I will write a blog about that and I thought today would be a good time, but I couldn’t find the words to talk about all the good things I learned. When I came home, the stress of everything that is going on drained me. I have a physiology lecture to watch, a module I could be doing, surg path notes I could look at, brain lecture notes from anatomy I should review before brain cutting Friday and 2 weeks’ worth of microbio lectures I could review. You get it I have a lot. Except today I came back tired and felt pretty down and I know my classmates feel this. We had microbio in person lecture get moved to all online which means I will have one lab and one lecture each week and the rest sitting by myself again in an apartment over zoom. I am thankful for technology to still allow me to finish this degree and to still be hands on in lab, but it feels discouraging being less than 15 weeks away from finishing didactic and over half my time in the program was spent learning alone. We cannot leave the state at this time because of quarantine rules and the stress of exams is starting to creep in. This program is not easy but trying to do this during a pandemic just doesn’t make it any better. This career isn’t easy, and I have seen PA’s work their butts off, leave the gross room to come back to their teaching desk and see emails that there are new rules for their students. I know that our professors are dealing with their jobs as our teachers, trying to do work in the gross work for patient cases and deal with the daily changes that come with teaching students online. All in all, we are tired because we are human and that is something everyone needs to remember. Be kind to one another, give professors some credit and give yourself a break. Go take a walk, take a nap or watch a movie. Talk to someone who knows your situation. I called up my friend Taylor tonight crying a little bit and we ended up laughing and talking about class and sometimes that’s all you need is to talk to someone who can relate. Be human and take care of your mental health because I’m learning that watching a lecture or doing something without full focus isn’t helping either. Pathology is the study of disease and for many, mental health problems is a disease and is just as important as physical health to take care of. Take the time off, drink water then get back in that game. I hope future students remember this time isn’t very glorious and there will be highs and lows but again, worth it if you keep pushing on.

SEE-FIM, see I Told You We’d be Back
Today I remembered why I wanted to be a PA. Not that I ever stopped of course, but in the midst of stress in trying to just learn as much information as possible to pass exams and survive the program, the parts of school that make you feel like you are job training and not just a student can be forgotten. Today I had a gross room rotation on day 2 of our return. What this means is that they allow us to work at a bench in Ruby alongside other PA’s and do real cases. They don’t hand you a big cancer case or anything, they want to get you used to the computer programs, working on dictations and using different instruments to practice how to cut. Practice is the only way to get comfortable mentally and physically at the bench. Sometimes it’s hard to explain the importance of the job and apply your knowledge but a perfect example came up today.
The PA helping me gave me fallopian tubes to gross with the preop diagnoses of wanting to prevent future pregnancy. To explain fallopian tubes and how they work attached below is a picture of a woman’s reproductive system. When sperm travels up the vagina and through the cervix, it then goes into the uterus. From the uterus it can travel into the left or right fallopian tubes. These tubes have projections called cilia to move sperm closer to the ovary. The ends of the fallopian tube are called fimbriae. These are finger like projections that sweep the ovary which contain a female’s eggs to pull the egg into the tube and sperm can meet with the egg for fertilization. Then the tubes help push the egg back into the uterus where the growing cells of the fetus can implant. You can see that removing the tubes would prevent sperm from reaching the eggs therefore to prevent pregnancy these can be removed. You can also see that failure of the egg and sperm to travel through the tubes back into the uterus can result in problems. This is known as an ectopic pregnancy when the cells of the fetus implant to grow somewhere other than the uterus. The most common place for this is in the tubes.

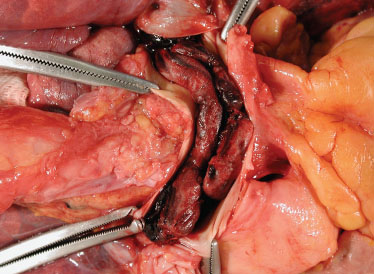
Back to grossing and why this information is important is because the way you handle this specimen changes based on what you need to show. If this is for a standard removal to stop future pregnancy you can cross section in intervals stopping at the fimbriae to bisect those. A couple representative sections can be submitted with half of the fimbriae in a cassette. Now, if the tube may contain an ectopic pregnancy serially sectioning may ruin the cut surface and what is inside. Therefore, opening the tube in a longitudinal plane to reveal possible tissue from an early pregnancy or sometimes even a small embryo can be discovered. In this situation you would need to show a section of the point of attachment and any early placenta-like tissue. Another situation that changes how you gross a fallopian tube is if the patient is BRCA1/BRCA2 positive. This gene mutation can predispose patients to developing certain cancer in areas such as the breast, ovaries and tubes , therefore a SEE-FIM protocol is used. Now cross sections are needed but instead of bisecting the fimbriae you need to have multiple thin sections to be thoroughly examined. The entire specimen gets submitted to review for cancer unlike the couple cross sections we would submit for a pregnancy prevention surgery. Everyday PA’s need to apply this type of knowledge to help aid in the diagnoses or treatment for patients, and PA’s do this with every specimen that comes across their bench. Every case is different, and I was excited to think of what knowledge I can keep applying in the future. I’m sure fallopian tubes aren’t exciting to a veteran PA but I hope I never lose sight of how important and cool this job is even with the little cases.
in order:
cross sections of a fallopian tube tube, ectopic pregnancy with tube opened to reveal evidence of a pregnancy, last picture outlines the sections needed for SEE-FIM protocol



I Went to Online Classes and all I Got Was This Lousy Mask
And we are done! A lot of exciting things happened over the last couple weeks of online classes and I finished up another round of finals. We finished Robbins textbook, 16 chapters of it in 12 weeks. They say read it through the first time so that it becomes a quicker, familiar reference in the future, so I am so glad to be done with the long, grueling first-time reading part of it. We are currently on our week-long break and I am anxious to see everyone Monday morning, 8am in the morgue. The school is handling the return of students safely and slowly and giving out some cool welcome back masks. We were required to get nasal swabs for our covid test and complete a module online. Most of classes that could be done online without labs are still online such as physiology. However, we are getting back into the morgue for autopsy and grossing practice, back to cutting frozen sections, back to the microscope room, back in for gross room rotations and back to surg path labs! Feels good to say WE ARE BACK!! A lot of busy days ahead and a really tough semester ahead. We are 15 weeks away from passing didactic year and getting onto rotations so there is still a lot to prepare for rotations such as dictations and handling more complex specimens and learning what to do at the bench in various situations. We are thankful and ready to get things back on track. Other great news! I have the honor of representing our program as a part of the AAPA Student Committee Public Relations Chair. This means I get to help create content for the social media pages. This is a great way to get involved with people from other programs, get involved with the AAPA, and also keep up on my knowledge of vocabulary and grossing guidelines. This is a great resource and if you are a future PA student I suggest giving them a follow on instagram, facebook and twitter! I am very excited for what is a head and I have a feeling I will have many new and interesting things to talk about on here.
Advice for the New “Future PA’s of America”
That’s what Michelle called us in her introduction email in January and it sounds pretty cool so I’ll steal it for a second. If you’re reading this blog looking for advice and some tips before coming in January, you should be super proud of yourself. This is a hard program, so you’ll want to remind yourself you love what you do because this emotionally and physically draining program is WORTH IT. So, I had some emails from people asking for advice and the first piece I can give is doing what you just did. Go to people for help. Ask the second years questions about how to deal with stress because we can relate so remember to keep me and others like our class president in mind. Don’t just ask us though, the most important people to go to will be your professors. They are also PA’s and very involved with other classes and grossing so be patient and make meetings to get help. They are probably ready to pass me on to clinical instructors by now so I can stop bugging them (just kidding!!) They are the best and would never turn you away. Ask questions during class and PARTICIPATE. You will be wrong, and pretty much everyone in my class has given a wrong answer at some point because you are learning just like the rest of them. In my Break it Down for Me blog I already talked about the Spring semester classes. I will say they are all hard. They should be though. I personally found AT was the hardest because I was an undergrad before this and hadn’t learned this type of info. Michelle’s exams are thought provoking and tricky and you may not do the very best on the first one, but don’t get discouraged go to her for help and spend time analyzing not just memorizing for that class. Others may have found anatomy and disease hard because they are older and haven’t taken those courses in years, I graduated last May so I was a bit more fresh than them. It all evens out so don’t compare strengths in that class just help each other out. So, here are some general tips I had to figure out worked best for me so do with this info as you please:
TIP: BUY A TAPE RECORDER. Seriously I never recorded a class in my life in undergrad. After the first exam I thought wow where the heck was that in my notes. Thing is, the classes are so fast paced, and you don’t even realize you have a question, or you missed it because you spaced out for a second and you don’t get that time back (especially AT). In my experience and maybe others don’t use this, buy a $30 recorder on amazon and bring it to class. It can’t hurt right? You don’t have to listen again if you feel okay, but I know some people go to the gym and walk on the treadmill and just listen. You will find some people make quizlets, flashcards, either study on their own or join groups. Each class I study different for, sometimes you read Robbins (buy your own Robbins textbook don’t rent) and memorize little mutations and names that seem like you can’t pronounce. Other classes I just stare at my notes figuring out how I can put myself in a real-life scenario. You will find what works for you. Your life will be consumed by this program and I mean that in the best way possible. You go in week one being like how do you gross a skin punch? Then all of a sudden, you’re learning how to gross a colon or head and neck specimen. You blink and this semester is over, and you know so much more. How cool is that?
TIP: INVEST IN A GOOD PRINTER. This is more of a necessity. The school computers are NOT great and you might have a lecture by a PA that was busy and uploaded the power point later that evening and you show up to campus next day to printers not working and you have to hand write your notes and all of a sudden you’re trying to draw a colon that has Crohns to reference later (think I’ve done this before?). So, you will print a lot you don’t type notes in class so, great investment.
TIP: PARKING PASSES ARE HARD TO GET. They give out parking passes to everyone in August who is lucky enough and it is good till July the next year which this doesn’t match up with our schedule. Undergrad, hospitals, we all have like the same lots so basically you can call in August and attempt to get a pass and not use it until you come in January OR!!! You can find street parking in the neighborhoods behind the Starbucks across from the building. A little bit of a walk but it is free and legal my friends and I have done it before. If you don’t have a car and plan to walk invest in an apartment near campus and don’t trust the bus system. Maybe bike there? Transportation sucks but if you do have a car find the free parking in those neighborhoods. Seems sketchy to not have a place to park coming in but that’s the truth everyone found their own way there.
TIP: TRY AND FOCUS AND TAKE THINGS DAY BY DAY AND TALK TO STUDENT AID FOR MONEY SITUATIONS. I had some people email me worried about rotations and how to find houses for those clinical days in second year, all that stuff. Funny thing is I don’t get my rotation schedule till the fall and I feel lucky to have even made it far enough into the fall semester with how stressful this whole spring and summer semester were so if I have to pay for a house for 6 weeks at a time I am up for it, no complaints just happy to be here! That’s not to scare anyone, it’s just you get a lot on your plate and you work so hard that adding stress about the second year before you start the learning won’t do you any good. You literally have to take it day by day week by week so try not to get stressed over rotations because you have to pass and focus on the first year first to learn as much as you can for those clinicals! They will let you know months before you go somewhere what your schedule is. I have no money of my own (for real) you cannot work during this program and my loans deferred from undergrad, I took out loans through those 4 years and through this year to pay for this apartment I live in now and all my books all that. My financial situation is a nightmare, but I can’t be the only one out there. If you have a husband or wife to help you or a job that you saved up some before you’re already in a better spot than me and I am doing it! I am lucky to get help from my parents with the small things, but they aren’t dishing out money for my graduate school. The school works with students, I take out graduate plus loans and they offer some scholarship and aid. Remember you signed up for grad school this part of school is optional, so they say hey you want a better paying job you’re gonna have to dish some more out first! School isn’t cheap but the pay for this career is great. Light at the end of the tunnel! You do have to pay for housing but there are a few locations that do provide it, so I am not 100% sure what they are. Things are always changing around here! Be prepared for that cost though I am still waiting to figure that out, but I bet the second-year students now would be willing to offer our class advice. It’s doable! You don’t pick you rotation spots they do, so it will be fun to see where I get to go and experience different hospitals and how different protocols are followed! I will try and post what I can later this year so you can follow along with that info. I know some classes have gone in on like a Pittsburgh house for the year and whoever rotates through sort of shares. There’s plenty of options that will all work out no one will let you live on the streets! I plan to keep up with the blog on rotations too so you can hear from me then. Don’t worry just take it day by day!
TIP: NO SCRUBS ALLOWED IN CLASS. They’ll give you the run down in orientation but as you pack up for school bring scrubs for cadaver lab, some EM labs and the gross room rotations, but for regular classes BRING NICE CLOTHES. Like you can’t roll out of bed and go to class. No ripped jeans sorry ladies and gents. I mean you can wear regular jeans and a tee shirt and closed toed boots or sneakers, comfy but not your PJs, no yoga pants either. I didn’t mind it I liked wearing comfy sweaters and jeans and my snow boots. You get a locker to keep your scrubs in to change in later for labs! Just be proud to represent this program dress the part is what I am trying to say! Pack an umbrella too. Lots of a rain sorry Cali or Florida people.
TIP: MAKE FRIENDS AND HAVE FUN!!! I will admit, they told us to have fun and get some sleep and rest and handed us our schedule and I was like oh you were kidding about that right? But you get to come up for air and we all used to get margaritas at Los Mariachis after exams. And classes are fun too you work hard and learn, and the teachers are passionate, so they keep your attention. It’s a small class and we all get along so make friends. Our class is awesome, I am one of the youngest and get along just fine with the people in their 30’s that have a lot of work experience because we all have a common goal: becoming a PA. Get together find what study group works for you or study alone go to the library get out of the apartment go for a hike. This is a quick year and my class was robbed a bit on the whole corona virus. But we still have a group message and face book group and send funny nerdy jokes. I think I found some life-long friends.
If I missed advice, please reach out to me I am willing to give whoever my phone number if you want to chat just email and reach out. It is scary taking the chance in this career, but you become a great student through this program, and I know one day I will be good PA and be jealous of all the first years that get to learn all this for the first time. Not jealous of the exams, but this experience is humbling and again WORTH IT.
PS. Follow the AAPA student committee if you have social media and join the face book group for path assistants! Just tell them you are an incoming student. I have learned a lot through social media and being involved in this community of PAs outside of WV too just another little tip to make things a little more fun.
Nausea Heart-Burn Indigestion, Upset Stomach, Metaplasia!
We’ve all experience that awful reflux of bitter fluid that comes back up after a chilly dog or one too many sips of alcohol. Our esophagus takes a beating with the hot liquids and acidic food we intake which is why our body is equipped with stratified squamous cells. Keratinized stratified squamous is the type of cells protecting the skin, which also takes a beating. So picture the esophagus with well-equipped cells, minus the hair forming keratin layer to withstand abrasion as food makes its way down. The point at which the esophagus meets the stomach is called the EGJ or esophagogastric junction. When food hits the stomach it needs broken down, which is why our stomach has secretory cells making pepsin and hydrochloric acid. Naturally, gravity doesn’t always keep the acid down, so where the protective esophagus meets the stomach at the EGJ cells are no longer stratified squamous cells, they become columnar and form mucinous glands to protect the esophagus from eroding its squamous layer if acid does come into contact with it. However, if you are someone with GERD or gastroesophageal reflux disease, the sphincter that usually keeps the food down relaxes too often allowing acid to splash back up out of the stomach. To compensate this constant exposure, the esophagus says hey wait, we need to make a change in cells, we need more mucous protection that the columnar cells can produce like the stomach makes. The point where the stratified squamous cells of the esophagus become columnar cells of the stomach is called the Z line. It sounds the same as where the physical esophagus structure meets the stomach, and in a healthy individual they are the same. However, in Barrett’s esophagus, the stratified squamous becomes columnar higher up into the esophagus even before the stomach. Therefore, the Z line and EGJ are not always the same. So, it might sound like this is a good thing, that your cells can adapt. But there is a reason the esophagus was meant to have its own cells. Barretts if left untreated can become dysplastic. Metaplasia means the cells have changed to normal looking cells in an abnormal location to meet a new function. But these mechanisms go bad quickly and produce abnormal cells called dysplasia which is a direct precursor to cancerous cells. Cancer that comes from those abnormal mucous, columnar glands is known as Adenocarcinoma. This can erode the layers of the esophagus and grow to outside structures such as the trachea. Treating Barretts early can lead to complete recovery if the acid is controlled, and squamous epithelium may return. Proton pump inhibitors like Prilosec or antacids like Tums have been useful in controlling acid reflux. On examination of the esophagus, the esophagus where stratified squamous cells are is seen as a gray mucosa, and where the mucous glands are as seen as red. In Barretts the red mucosa replaces that grey in the esophagus as pictured before. It is important to note where the Z line is in relation to the EGJ and also if and tumors are located if they are near the Z line and EGJ. Doctors must decide how to stage a cancer if they will use an esophagus or stomach protocol based on the tumors center point from the EGJ if it’s more in the esophagus or more in the stomach.



Von Meyenburg complexes? Sounds like a Buzz Word to me
It only took about a week in the program to realize that some terms in pathology have some pretty funky names. There are special names for just about everything. It can be overwhelming trying to even say the right term or spell it, so remembering what these terms mean and what mutations are linked to them is making the future boards exam sound even harder. I said before I was starting to keep a running tab of flashcards for each chapter in stem path and it really seems to be helping! I wanted to give an example of what I mean by funky names of some these syndromes. Last chapter we learned about the GI system. When a tumor metastasizes to a woman’s ovary it’s called a Krukenberg tumor. Like my teachers say, “probably named after the guy that discovered it”. In the liver chapter, and in AT last semester we learned about the hamartoma known as the Von Meyenburg complexes. A hamartoma is a disorganized growth of tissue that is indigenous to that organ. This hamartoma is a disorganized growth of ducts. My favorite so far has to be the lines of Zahn. When a person dies and blood comes to a stop, in autopsy you can find post-mortem clots, which means the blood clot did not have to do with their death and formed after their systems shut down. So how can you tell the difference from a clot that was fatal and a clot that formed after death? Well, under microscopic exam a suspected clot that formed when the person was alive had to go through the process of the coagulation pathway to form the clot. This involves fibrin, platelets and red cells coming together in the pathway. Often these clots can move from their originally formed site and travel to places such as the heart and can lodge in the lungs. If you look at a clot under the microscope and see alternating bands of fibrin, platelets and red cells, these are known as lines of Zahn. Post mortem clots have a yellow, rubbery consistency like chicken fat and don’t have this pattern. A lot of people have heard of DVT’s on commercials. This is called deep vein thrombosis whenever you have poor circulation and blood is stagnant in the legs. A clot may form and when this thrombus moves, it is known as an embolus. When the embolus is too big to fit through vessels it can stop and block the blood flow. Often DVT’s travel to the heart and into the lungs and stops at the bifurcation of the pulmonary arteries causing pulmonary embolism. The clot causes death in minutes and is known as a saddle embolism. So next year if you’re in the program, remember to write down these funny terms, because you’ll see them come up a lot in this field!

/GettyImages-578458001-566c1bf45f9b583dc34ce45b.jpg)


Is Going Back to School After Working for Awhile the Right Move?
Well, I guess I can’t answer that question myself. Some people are lucky enough to work in different areas of this field before deciding being a Pathologists’ Assistant is for them, but some are worried about leaving the security of a paycheck, taking on more student loans and getting back into hitting the books. I decided to interview some of my older classmates who have experience as a Medical Laboratory Scientists, a Path Tech, and an uncertified Pathologists’ Assistant. So if you’re looking to get some advice and hear about others’ experiences leaving their jobs and entering the program this post is for you. This is what 3 of my fellow classmates had to say:
Advice from a Medical Laboratory Scientist:
What were you doing before PA school?
I was an MLS for 5 years, charge tech on night shift.
What made you want to come back?
I was continually stressed out and bored with my job. It was starting to get monotonous. I wanted to do something where there’s more thinking involved. I’ve always liked pathology, it seemed like a logical next step for me. I’m artistic and detailed and I liked that I could use that side of my brain more. Less cog in a machine, more autonomy.
What were some fears about coming back to school?
There’s a lot of debt, and I had paid off my undergrad debt before I came back to school. Taking on massive debt again is kind of scary.
Was the program what I expected?
Yes and no. Yes, it’s very difficult, everyone will tell you that before you start. I didn’t expect to make new best friends from this. I didn’t expect the professors to be so excellent. (Honestly, they’re great) I expected to be pushed. I didn’t expect I’d enjoy it as much as I do. I would 100% make the same decision again. I loved doing the gross room rotations. I love that I’m excited about my future job, where before it had gotten to the point I was so burnt out.
What’s the most challenging part as a person with experience?
Time management and finding ways to destress. Specifically for my class, taking online classes for Covid has been a real challenge, but we’ve adapted.
What areas did I struggle with?
Anatomy is the only class I’ve felt was extremely difficult for me. There is so much information. I had never previously taken anatomy, so everything was new. The cadaver lab was excellent though- I throughly enjoyed doing the dissections and it helped a ton with memorizing things for lecture.
What areas has my experience helped with?
My MLS background has been very helpful, especially in disease class, and obviously in clin lab. It’s helpful to have context for what you’re learning. Robbins sometimes throws random test values at you, and it’s nice that I know what they mean. We learned about several of these diseases in MLS school. Clin lab is an easy class for me, which is nice. Also, general familiarity with a microscope is helpful. It helps out with microanatomy.
Advice for people in the medical field who are thinking of applying?
Shadow, shadow, shadow. Try to shadow surgical and autopsy. That’s the only way to figure out if this is for you. I find PA to be more interesting than MLS, but maybe you wouldn’t, and that’s ok. I’m happy in my decision, and I think it will pay off in the long run both financially and with quality of life.
Advice from an Uncertified Pathologist’s Assistant:
What were you doing before PA school?
I received my Bachelor of Science degree and had been applying for jobs around North Dakota. There was a job opening for an uncertified pathologist’s assistant at a local hospital. Although I did not know what a pathologist’s assistant did, I was eager to learn. I met all of the requirements, did great in my interview, and got offered the position. I started working in the Histology lab first then trained in the gross room.
What made you want to come back?
After working as an uncertified pathologist’s assistant for 2 years I really enjoyed what I did and wanted to advance my pay or position. The only way to do that was to become a lab supervisor, but that position was not open, or go back to school to become certified and make double what I was making. I was doing something I thoroughly enjoyed, so going back to school seemed like a great idea.
What were some fears about taking the leap and going back to school?
My biggest fears were moving across the country alone, not being able to pass the classes, and the debt I was going to take on. Before going back to I recommend you calculate your financials so when you graduate it is not such a burden of a debt. Even though you will be making good money, it is a stressful situation too.
Was this program what you expected?
Yes, the program at WVU is what I expected and more. They prepare you to take your board exam through their teachings in class and exams. You get hands on learning of anatomy in a cadaver lab. They have the students on gross room rotations to learn how to gross specimens. I really enjoy the labs we have in the morgue, and think it is great that we have the opportunity to learn in there.
What is the most challenging part for you as a person with experience back into the college setting and what areas do you think you struggle with in the program, and what areas has your experience helped you with?
I have been out of college for 5 years, so it was very challenging and stressful to figure out how I study best. They truly cannot prepare you for the stress of this program. You hear people say Masters programs are stressful, but until you are in it you don’t really know what that stress is. You just have to always remember the end goal and why you chose to be in this program. You didn’t get here by luck, you were specifically chosen out of many people. Be proud of yourself. Even getting an interview is such a huge thing. You worked your butt off to get where you want to be, so once you are in the program you will keep working hard. When was stressed out and worried, our program director Michelle was there to talk to. She is a great listener! All of the teachers and PA’s have been through the same thing we are. I was not scared about meeting classmates and gaining new friends. That is the fun part of it! Your classmates become very close to you, almost like family. You do a lot of things together and rely on each other for so many things even outside of college. I learned how to keep working hard even when you feel like it is too much. It is such a great experience and not everyone gets the chance to do it!
Any advice for people in the medical field now who are thinking of applying?
Decide if this is what you really want to do. Get experience by job shadowing to learn what a PA’s day looks like. It is a great career and it will never go away. Some days can be very stressful for a PA so know if you handle stress well. You are a very important step in someone’s life outcome as far as treatment goes. That is what is most rewarding! You are helping patient’s kind of behind the scenes but in a very big way. You should definitely apply if it seems like something you would enjoy after job shadowing. A big thing is to not give up if you do not get into a program the first time applying. I have heard of people getting in on their 2 nd or 3 rd try. Most programs do not take that many students. Your chances of getting in the second round are much higher. Practice for your interviews, know some basic interview questions and be prepared to answer some tough questions. It is okay to ask for a second to think before you answer. Just be you and smile! They are looking for something special in you that makes them believe you would be great for their program, and more importantly a great PA!
Advice from a Path Tech:
Before PA school I was working as a pathology technician in the gross room. My main job was accessioning patient specimens, but I was also responsible for patient send-outs, going to intraoperative procedures (Thyroid FNAs, and Endobronchial/Endoscopic FNAs), cutting frozens, staining slides, ordering special tests, and a bunch of other random things.
I knew I wanted to go to PA school when I received my job as a path tech. I had worked as an autopsy tech and heard about PAs through work/google. I knew I would need shadowing/work experience in surg path and started looking for opportunities in the field.
My biggest fear with going back to school was the finances. I am thankful to have a husband that supports me while I take out hefty loans to pay my tuition. I remind myself constantly that with the 100% job rate WVU has I will be paying the loans back in no time.
As a person who has worked in the field I feel very confident in my autopsy dissection skill, but having been out of school for three years I worried that I would struggle to remember my in-depth anatomy/physio courses. It definitely took some extra studying, but my mind was refreshed when we covered the topics. Probably the biggest thing my job experience helped me with was already knowing the pesky CPT codes you will have to memorize as part of Anatomical Techniques.
To anyone already in the medical field considering applying I say go for it. Definitely know what you are getting into though. Make sure you have shadowed and know ALL the aspects of being a PA. Contrary to what you usually see, we don’t just gross specimens. Haha The PA field is made for people who love to be hands-on with anatomy and love to see the gross and crazy cases. If you are thinking of applying to this program as a stepping-stone to something else…this is not the degree for you. If you would rather be working with the specimen than looking at the microscope slides, go for it!
Anatomy + Disease Mechanisms + Anatomical Techniques = Systemic Path
I’ve been a bit absent on the blog lately, so I intend to keep up more this summer, I just don’t have the hands-on cool stuff to talk about anymore! But we’ll make do if you’re tuning in still. I’ve gotten some emails from interviewees about my previous Interview blog post. Shoot me an email with questions I’d love to chat about the program! (kelsiebalsam@gmail.com). Anyways, I thought I should give an update on what PA school online has been like. We finished up finals and that week was a nightmare. Not to be dramatic but cumulative finals should be added to the list of underlying causes of hypertension. There wasn’t much sleep going on and a lot of coffee. But here I am, on the other side 2 weeks into summer session already. My week long break was spent well, doing nothing. I felt invincible when I passed last semester and it gave me hope that this isn’t impossible, and our professors are really rooting for us, I can’t stress that enough. Here is what we have going on in the summer now. We have path 750, a continuation of Robbins chapters. Now we are focusing on systemic pathology. Path 650, Disease Mechanisms involved overall mechanism. For example, if you have a cut, and you start to bleed at this injury site, what types of cells would be involved, why do we clot and what genetic mutations are common that would make it hard to clot. So, systemic path kicks it up a notch by going organ system by organ system on what diseases affect that tissue specifically. Week one was about the liver, so we learned about Hepatitis, Cirrhosis, and alcoholic fatty liver disease which as our professors like to point out, we all have a bit of that from quarantine drinking. Basically though, this course involves grossing techniques and CAP checklists and recalling anatomy both gross and microscopic. If AT, Disease, and Anatomy (all of the courses from last semester) got together to make a baby, it would be called Systemic Path. So yes, this course is HARD so far. We have one other class which is Clinical Pathology, which talks about more of the living patient aspects of disease. During autopsy especially we may need to read charts about patients that were in the hospital and what glucose levels looked like in kidney failure, urinalysis and normal vs abnormal levels could aid in post-mortem diagnoses. Yes, this class is kicking my butt already. It sounds like a lighter workload since we only have 2 courses instead of 4 like last semester, but I assure you the complex material really keeps you just as busy. I started making flash cards for names that could be on the boards as I go along in Robbins as our director suggested. If a Von Meyenburg complex or Caput Medusa question isn’t on the board’s exam, I’ll be highly disappointed! Learning online has been difficult. You feel like you stare at a computer all day and Robbins textbook starts to blur, but you just learn to be disciplined and enjoy zoom meetings when you can. This is grad school, so a lot of this stuff would’ve been done on our own time, quarantine or not. Advice for next year’s students, don’t take for granted class time, open lecture conversation because our teachers make it fun, and even those 8am doctors conferences. I’d do anything to be in the morgue practicing! I’ll be tuning in when I find something really interesting in Robbins. Until next time, stay safe!
Polio vaccine helped us walk, literally, so Covid-19 could run
This blog is going to be a little different for now, since there won’t be many specimens I can discuss for the time being. Yes, the program is being done online all summer too and yes, everyone is disappointed. I miss my classmates and our celebratory margaritas after the exams at Los Mariachis (don’t worry I still FaceTime my friends after to stress about what I think I got wrong so going about things normally)!! I am missing class discussions tho and actually was starting to understand what the Path residents were talking about in conference. Our director and other professors have made this a smooth transition, but we miss the cadaver lab and hands on aspect of our training. But with that being said, we adjust like the rest of the world has and we’ve been so busy that even if we were able to leave the house and go out, we really don’t have the time to. This semester flew by to say the least! Ironically over spring break a couple weeks ago we were learning a chapter in our Robbins text about viral mechanisms such as Measles, Mumps, Polio and how, many of the issues we faced with these viruses were eradicated because of our understanding in the health field about how viruses invade since not all work the same. Which is probably why we hear of how fast people have worked to come up with vaccine trials for Covid-19 and can quickly understand how this virus spreads, attaches, and works its way into our system. With advanced technology and our quick understanding combined, I bet over the next few years the next generation of PA students we will be reading about the virus in our Robbins as we do now about other viruses that once wreaked havoc. So, in the midst of the craziness I figured I could talk a little bit about how some viruses find ways to work around our immune system and why they are difficult to treat. The PAs teaching us always say these are great board questions, understanding the receptors and common names and proteins involved. In our disease mechanisms course, we learned about the pathogenesis of HIV. HIV (human immunodeficiency virus) is a virus that attaches to our body’s own immune system cells called helper T cells. Helper T cells have receptors on the surface called CD4 and CCR5. Normally these receptors are ones that can attach to our own cells to say “hey we have a foreign substance that needs killed, let’s bring in more of our immune system and get cells to come eat and break down this bad thing and make antibodies so we recognize this if it comes back.” So, HIV is this virus that has a protein called glycoprotein 120 that can trick the Tcells and allow it to fit perfectly into the receptors CD4 and CCR5. Once this happens another protein called gp40 on the virus causes the membranes of the Tcell and the virus to merge together opening up the Tcell to the virus. The virus itself gets digested inside and the RNA of the virus which is its own genetic material from the gp40 gives instructions and plants itself into the host’s genome. Our own Tcells have instructions in RNA to make DNA which tells the Tcell how to function properly. So, if the instructions to get a Tcell to recognize a bad cell is a code like “GCCA”, viral RNA inserts its own instructions to say, now your new code is “GTTCCA” (this isn’t actually the code this is just an example of how it changes functionality). All of a sudden you have a Tcell that isn’t able to do its own job because it is working under the new instruction of the virus, often times it tells the cell to die and self-destruct. If you have a different virus or bacteria come into your body, your Tcells are too busy dying off and won’t be there to tell your immune system to bring in those cells to fight off this other infection. That is why this virus causes AIDS (Acquired Immunodeficiency Syndrome). This virus ruins your body’s line of defense so secondary infections that normally wouldn’t be an issue and could fight off can take over the body and invade. These viruses are so difficult to treat because every time the virus spits new RNA into the gene, it changes the code and varies in instruction making it unstable and unpredictable to follow and eradicate. In people with AIDS, the virus goes latent and hides until the Tcells need to go do their job and all of a sudden, they can’t because of the variable mutations. During this pandemic a virus such as Covid-19 could be even more harmful to people with immune deficiencies such as AIDS. This program really helps you become well rounded and better educated so we are able to apply and comprehend the world around us. Next time, I think I’ll explain the process behind frozen sections. We were going to be practicing them this summer, so until next time! be safe and wash those hands.